ICU tower shifts to team-building, quality, safety culture
Published on Thursday, September 20, 2018
By: Ruth Cummins
When Dr. Hartmut Uschmann began work more than 20 years ago as an attending physician in the University of Mississippi Medical Center’s intensive care units, some employees there were barely civil to each other.
“We almost had hostilities between the ICUs, driven by the faculty and the chairs of the departments,” he said. “The ICUs were more siloed by floor and department.
“The collaboration between ICU providers is the basis for collaboration between the ICUs. Somebody’s got to start the process.”
Uschmann and a number of the Medical Center’s newest critical care providers are doing just that, changing the culture of poor communication and too little camaraderie to one of cooperation and idea-sharing. “There’s more of a grassroots approach,” Uschmann said. The divisiveness, he said, “has completely gone away.”
The different approach is guided and encouraged by hospital administration as providers bear down on improving quality measures and reducing harm through “Chasing Zero,” an effort championed by The Joint Commission that strives to eliminate serious safety events and cultivate safer, more effective patient-centered care.
The culture shifts and the gathering of quality data are key to achieving goals that at the end of the day boil down to a single focus: the best outcome for the patient.
“We need standardization of staffing and protocols. We need engagement as part of improving outcomes,” said Dr. Michael Henderson, chief medical officer. “If you can do that, you can really improve outcomes.”
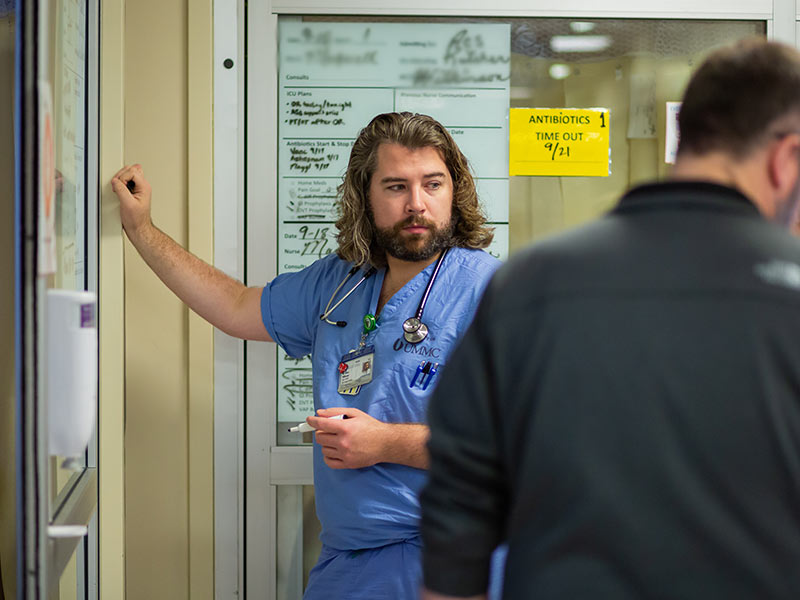
 Dr. Matthew Kutcher, center, leads rounds in the surgical ICU.
Dr. Matthew Kutcher, center, leads rounds in the surgical ICU.Dr. Jay Shake, professor of cardiothoracic surgery, is medical director of the Wallace Conerly Critical Care Hospital, which houses the medical, surgical, cardiovascular and neuroscience ICU units. Shake, who also is medical director of the cardiovascular ICU, is shepherding change hand in hand with Uschmann, professor of neurology and NSICU medical director; Dr. Andy Wilhelm, associate professor of pulmonary medicine and MICU medical director; and Dr. Matthew Kutcher, assistant professor of trauma and critical care surgery, and Dr. Hess Robertson, assistant professor of anesthesiology, co-medical directors of the SICU.
They’re talking to each other. A lot.
“We’re having discussions, not just on a unit level, but on a tower level,” Shake said. “Are we seeing pockets of infections? I get emails on what floors have gotten what infections, and we look to see if there are patterns that we can work on. We track it, and we look at it.”
“If you don’t talk to each other, then you don’t get anywhere with standardizing anything,” Uschmann said. “Now, there’s more buy-in. In the past, it didn’t go beyond (just one) ICU. Now, when someone comes up with something that can be improved upon, they send a group email and everyone chimes in.”
They also come together on what’s good for the patient, regardless of what ICU floor you’re talking about, and sometimes regardless of which physician has charge of what patient.
“We’re beginning to notice that you have to go up or down the floors to find the expertise that you might not have, and to use the best tools in the whole building,” Kutcher said. “If we have a patient in the surgical ICU with critical respiratory issues, we go upstairs and talk to the pulmonary folks. If we have a patient with a cardiovascular issue, we might walk upstairs and talk to Jay Shake.”
 Kathleen Lovelace, right, a pharmacy student, joins students and front-line caregivers making CCU patient rounds.
Kathleen Lovelace, right, a pharmacy student, joins students and front-line caregivers making CCU patient rounds.The Medical Center has made great strides in hiring to ensure quality and safety on all shifts, Uschmann said. “It’s not possible to produce quality in an intense ICU setting, with very complex patients, if you don’t have the manpower to make it happen,” he said.
Safety and harm events, Wilhelm said, “are related to process breakdowns. If all of the steps in the process aren’t outlined, and people don’t have accountability for the steps, or if we don’t have enough people to do the steps, we’re setting up the patient for harm.”
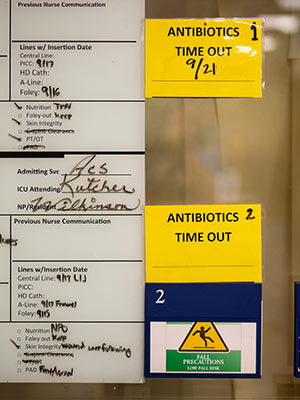 Signs on the doors of surgical ICU patient rooms give safety and treatment instructions and spell out chief caregivers.
Signs on the doors of surgical ICU patient rooms give safety and treatment instructions and spell out chief caregivers.Robertson said one of the biggest and most necessary shifts is driven by attitudes, not just process. “The culture shift has been away from the ego-driven ‘I know everything.’ Attendings in the past have maybe had the mindset of ‘I don’t want to be questioned.’ If you include everyone on the team in the process, then the patient gets better care,” he said.
When ICU attendings round by patient rooms, they review information on communication boards posted on each door. They hold a collaborative discussion with residents, nurses, nurse practitioners, pharmacists, medical students and others in the rounding group.
“Multidisciplinary rounding is absolutely the standard in critical care medicine, and we’re quickly moving in that direction,” Wilhelm said. “We’ve been doing this for three or four years. The medical directors now in place are all on the same page.”
“It gives the culture change a daily presence. People are taking ownership of this,” Shake said. “The nurse can say, ‘Can we get that catheter out today?’ It raises a new level of awareness to be ingrained into our residents and students.”
 Dr. James Wilkinson, left, emergency medicine resident, prepares to write notes on a patient's "communication board."
Dr. James Wilkinson, left, emergency medicine resident, prepares to write notes on a patient's "communication board."On Tuesday, Shake made rounds with two nurse practitioners, a medical student, a pharmacist and a pharmacy student. He was managing care not just with the rounding group, but with input from physicians who aren’t his patients’ attending.
“I talked to Pierre (de Delva, chief of the Division of Thoracic Surgery) about this patient,” Shake said at the room of an individual coping with esophageal challenges. “He’s going to talk to the family about what they want to do.”
Making rounds Tuesday with Kutcher was charge nurse Morgan Self. When she began work in 2011 on the SICU night shift, Self said, “it was definitely intimidating not knowing the doctors or attendings. Now, the doctors make an effort to say, ‘Do you need anything from us? Is there anything going on with your patient that we need to know about?’”
 Youngblood
YoungbloodHospital administration and the ICU medical directors give Shake much of the credit for building relationships between physicians and other front-line staff. “It’s just one example of the work across the organization to elevate and promote patient-centered care,” said Liz Youngblood, CEO of the adult hospitals and metro-area clinics.
“We look to Dr. Shake and our medical directors in the ICU and elsewhere to provide us with their recommendations on how best to provide care, whether that be from a staffing perspective to a standard of care, to a specific practice or competency,” Youngblood said. “They are the ones who tell us how to support excellent patient care. Our job is to help them make that happen.”
Two years ago, Kutcher interviewed at UMMC following a trauma and acute care surgery fellowship at the University of Pittsburgh Medical Center. “The person who articulated the vision of expanding the role of critical care, and looking to collaborate more across different specialties, was Jay Shake,” Kutcher said.
About the same time, Robertson came on board after his anesthesiology critical care medicine fellowship at the Cleveland Clinic. “We all know how to take care of sick patients, but a lot of the things that go on in each ICU unit are the same,” he said. “There should be standard best practices, and we’re getting there.”
For four years, Wilhelm has worked in the trenches with Shake to help prepare for process improvement, implementation and adherence. “Now, we’re optimizing the processes and personnel to take advantage of the positive energy and the institution’s focus on patient safety and Chasing Zero.”
“There is no doubt that we’ve had an evolution over the last couple of years,” Shake said. “The next step is even more nurse empowerment. This is a team effort, and that can’t be stressed enough. The barriers are being taken down. We’re heading in the right direction.”